|
Plantar Fasciitis & heel pain The most common cause of heel is Plantar Fasciitis or chronically known as Plantar Fasciopathy. The Plantar Fascia is a thick band of tissue that runs across the bottom of the foot originating from the heel and attaching into the toes. The Plantar Fascia provides support into the arch of your foot with other ligaments, tendons and bones. This is critical for the support of our feet with weightbearing activities that we perform through our everyday lives. Excess stress to the Plantar Fascia can cause micro tears and lead to injury. These repetitive micro tears result in the catalyst for the development of Plantar Fasciitis. Some examples of excess stress can be:
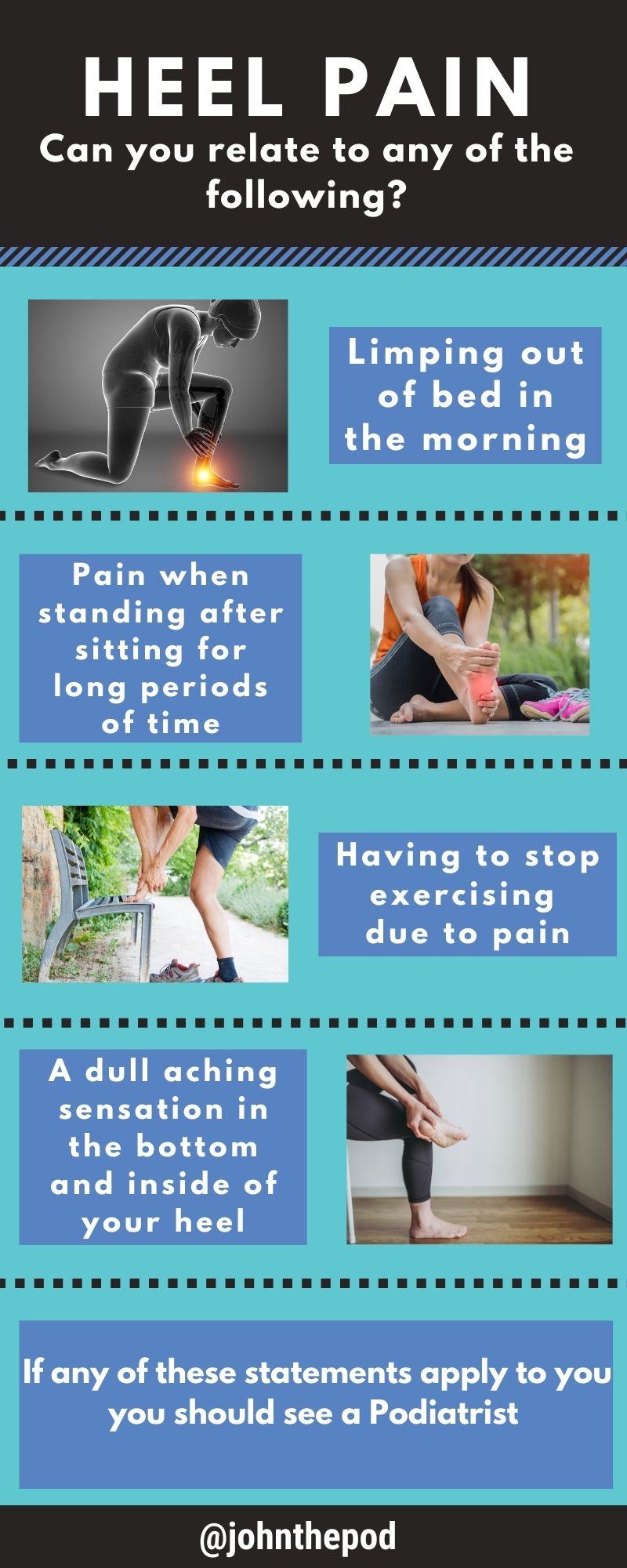
Most common symptoms include:
Treatment for Plantar Fasciitis can consist of:
|
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
April 2024
Categories |
|
|
|



 RSS Feed
RSS Feed