|
World Continence Week 2021 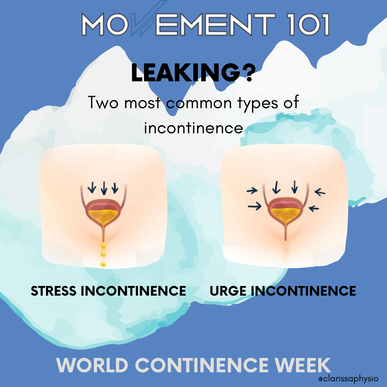 The 2 most common types of Urinary Incontinence are: Stress UI Loss of urine associated with an increase in pressure (e.g., cough, laugh, jump) Urge UI Loss of urine associated with a strong sense of urgency 4 ways women can reduce their risk of incontinence Staying active
Research suggests women who are active have lower levels of incontinence and stronger pelvic floor muscles. Physical activity can also help prevent constipation, helping reduce incontinence. See a Women's/Pelvic Health Physio Women's health physios can diagnose and treat incontinence. They can also help you prevent it! A physio may recommend pelvic floor exercises, teach good bladder/bowel habits, offer lifestyle advice, and advise on exercise. Check your beverages Try reducing your intake of caffeinated, sweetened, & alcoholic drinks to see how your bladder responds. These drinks are known as "bladder irritants" and can make symptoms of urinary frequency and urgency worse. Maintain a healthy weight range Research has shown increased body weight increases incontinence risk. Losing body fat may help significantly reduce incontinence symptoms. However, fat loss is not a healthy goal for all women - especially those who have disordered exercising or eating history. For those women focus on the previous 3 strategies above. If you have been having any trouble with leaking book in with our Womens Health specialist Clarissa Yiu Fungus  What’s a topic you don’t hear men speak about too often? Their foot health perhaps??! Something that can be quite prevalent amongst men but not regularly spoken about is skin and nail fungus. The idea of scrubbing our feet in the shower or applying cream almost sounds outlandish right? As a Podiatrist and a foot nerd, I wanted to highlight this condition and provide some simple tips to prevent this from occurring. Condition 1: Athlete’s Foot Athlete’s foot is a skin infection of the foot due to a thing called “dermatophyte fungus” which typically presents itself in the soles of the feet and in between the toes. Athlete’s foot will usually present itself with dry, itchy & scaling skin. In more severe cases, it can also cause inflammation, cracks & blisters also. Infection is usually acquired by direct contact with fungus, for example, walking barefoot in a public change room. Other risk factors include: occlusive footwear (work boots, steel caps), excessive sweating, immunosuppressant medications, showers & sporting locker rooms. Simple prevention & treatment
Condition 2: Nail Fungus (onychomycosis) Nail fungus is a fungal infection of the nail bed, matrix (the area where your fingernails and toenails start to grow) or nail plate. Nail fungus causes discolouration, thickening and separation from the nail bed. The cause is similar to Athlete’s foot but with the fungal infection affecting the nail rather than the skin. Nail fungus is often harder to treat than Athlete’s foot and can persist for months sometimes even years, so prevention is key. Prevention is the same as Athlete’s foot however there a few key differences in treatment. Keep in mind, nail fungus is more stubborn and likely to hang around longer so if a particular nail treatment is unsuccessful after a few months then you should switch to another one. It could take up to 18 months to fully resolve so be persistent and consistent! Simple prevention & treatment
Lateral elbow tendinopathy, also known as lateral epicondylitis is the technical name for tennis elbow. It is a condition where there is pain and or swelling in the forearm extensor tendon on the outside of the elbow. Patients will normally have pain with lifting up the wrist and fingers and report difficulty gripping or holding objects. If it's mild, you may only feel symptoms with certain movements involving the arm and wrist. However in more severe cases, pain can be constant which disrupts sleep, interferes with work and persists for a long time.
What’s the cause? You may have caused a tear or irritated this tendon from overloading or overuse. It can be due to sports mainly racquet or throwing sports. But more commonly,we see this condition with repetitive work for people like plumbers, painters, butchers, carpenters, hairdressers and computer workers. It can also be from excessive lifting, carrying, gripping and poor arm strength or technique. What can I do? What are the treatment options? Firstly, rest. If you can modify or stop doing the repetitive activity that’s aggravating you, it might just get a chance to heal and your symptoms will improve. Unfortunately, tennis elbow may not completely resolve with just rest so I would strongly suggest working with a physiotherapist for the best outcomes. The literature recommends conservative management as the first line treatment for tennis elbow. Some people opt for an elbow or wrist brace for support to improve pain and function in the short term. However, there is no clear indication in which splint or brace is superior and there is very low evidence for whether it’s beneficial or not as an adjunct to treatment. Exercise - There is strong evidence for exercise as the ‘ideal’ treatment for tennis elbow, whether it be exercise alone or in conjunction with other modalities. Most practice will use a combination of physiotherapy treatments (joint mobilisations, manipulation, massage, taping, etc) and exercise for a more positive response amongst patients. Although there is no consensus on a specific type, frequency, duration or intensity of exercise, the general guideline is to target the wrist extensors with a progressive strengthening and endurance exercise program. How long will it take to recover? If picked up early, you can definitely see improvements in a 6 week course of physiotherapy, (some studies have noted up to 60% improvement). If left untreated, it can take more than 6 months to 2 years for recovery. People who present with higher pain levels and disability at baseline are more likely to still have pain after 1 year. Additionally, those who report shoulder and neck pain with tennis elbow had poorer prognosis in the short and long term. Patients who do lots of manual or office work involving repetitive arm and wrist movements may be more resistant to treatment and take longer to recover. Some helpful exercises: (please refer to video) Isometric WE: Isometric contractions - this is a good starting exercise to help provide pain relief, by tensing the muscles on the forearm, you can use your other hand to add a bit of resistance. This has been shown to provide some pain reduction. Hold for at least 1 minute and try to do at least 10 reps. Ball squeezes: Hold a soft squishy ball, (you can try socks, rolled towel or putty) in your hand and squeeze the ball gently, hold for at least 5 seconds and aim for 20 reps. This will activate the forearm muscles and help improve grip strength. Wrist extension with DB: Have your arm resting on a bench, grasp a weight with an overhand grip (palms facing down). Raise the dumbbell up (wrist extension) and then slowly lower the weight all the way down. Try to do 10-15 reps. Supination with DB: Hold the dumbbell at the bottom, rotate the dumbbell so that the thumb turns outwards, palms facing up. Rotate the hand back the other direction until your palm is facing downward. Repeat 20 times on each side. |
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
April 2024
Categories |
|
|
|



 RSS Feed
RSS Feed