|
Most tissues in the body have healed completely in six to 12 weeks following an injury, however, many people have severe pain that lasts much longer than this. We know that the intensity of the pain you feel is not always associated with a similar amount of damage. In some cases, there can be a severe amount of pain with almost no detectable damage. With this in mind, we explore some reasons why your pain might not be getting better, long after the tissues have healed.
You’re afraid of the pain.
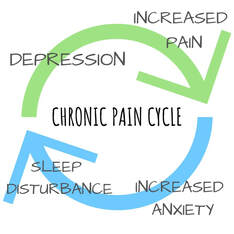
Pain can mean many different things, for some of us pain can affect our ability to work or can be a symptom of a serious disease. What you believe about your pain can either amplify or reduce the symptoms you experience. If you feel that every time you experience pain you are causing more damage, you will naturally pay more attention to this and your nervous system will amplify the signals in an attempt to keep you safe. If you understand the cause of your pain and know that while there is discomfort, you are not in danger of causing more damage, often the pain will feel less severe. This is one of the benefits of seeing a physiotherapist after your injury as they can help you to understand your pain, giving you more control over your recovery. You started moving differently after the injury. Immediately after an injury, it’s natural to change the way you move to avoid painful movements. After a while, these changed movement patterns can become maladaptive and actually begin to cause pain and discomfort on their own due to the altered stress patterns placed on your body. Correcting these adaptive movement patterns can often go a long way in reducing pain after an injury. You might not have noticed these changes and might need a physiotherapist to identify and help you to return to your usual movement pattern. You have lost muscle strength since the injury. While a certain amount of rest following an injury is always helpful, if we stop moving altogether, our muscles can lose strength. This can mean that our posture changes, we fatigue easier during our usual activities and that we are more susceptible to further injury. Less movement also means we actually focus on the pain more when it does happen. Physiotherapists are able to advise you on the right types and amounts of excercise for you in the period following your injury. The pain has affected your lifestyle. When pain affects your ability to sleep, work and even concentrate, it’s not surprising that this can have a negative affect on your overall wellbeing and mental health. This can create a negative cycle of anxitey and depression that perpetuates and increases the experience of pain. If your pain is really getting you down, speaking to a mental health professional can actually be a valuable part of your physical recovery.
What is an Achilles Tear?
The Achilles tendon is a band of fibrous tissue located at the back of the ankle. Its main role is to connect the calf muscles to the heel of the foot. This tendon is the largest tendon in the body and when it tightens, as the calf muscles contract, it pulls the heel allowing you to stand on tiptoe or to point your foot. Achilles tendon tears commonly occur in athletes, however, this injury can affect anyone and surprisingly, a complete tear is actually more common than a partial tear. These tears are commonly located at the part of the tendon where there is poor blood flow approximately 6cm above its attachment to the heel. Since there is poor blood supply, this part of the tendon is both vulnerable to injury and slow to heal. What are the symptoms of an Achilles tear? Primarily, an Achilles tendon tear will cause difficulty in activities such as walking, running and jumping. Other signs and symptoms of an Achilles tendon tear include:
What is the cause? Anyone can tear their Achilles tendon if the tendon is subject to excessive force or overstretching, however there are some factors that can increase your risk of injury. The most common activities that cause this injury are running and jumping. The Achilles tendon can thin and weaken both as we age and also if it is not used. As a result of this weakening, it becomes prone to injury like tear or rupture with less force or stretching required before an injury occurs. A tear of the Achilles is often observed in people with pre-existing Achilles tendinitis. Other factors such as certain medications including antibiotics and steroids and some illnesses like diabetes and arthritis can also result in weakness of the tendon, increasing injury risk. Being obese is also a risk factor as excess weight puts additional strain on the tendon. How can Physiotherapy help? Treatment for Achilles tendon tear will depend on the patient’s age, how severe the injury is and the patient’s activity level. For young people especially athletes, they opt to have surgery while older people choose conservative treatments including physiotherapy. Physiotherapy treatment for an Achilles tendon tear will involve exercises to strengthen the calf muscles and the Achilles tendon and exercises for stability. Many people are able to return to their normal activities within 4 to 6 months. Functional rehabilitation is also part of the program as it focuses on how you coordinate your body and how to move it. The aim of functional rehabilitation is to help you return to your highest level of performance.
One of the common complaints that we hear from our clients is they often feel they have a limited range of movement in their shoulders and tightness across their pec muscles. Here’s a few simple exercises for you to try next time you experience the same issue. . . . Long, deep breaths into your abdominals will help facilitate a smooth movement pattern. Be mindful to keep your spine and pelvis in neutral position. The roller provides a nice feedback for your shoulder placement, as well as challenging your stabilisers to maintain balance. Any imbalance in strength and mobility between the 2 sides can be easily identified. To progress the exercises, you can increase the weight used. Enjoy the lovely shoulder release! ?
Let's talk about ankle sprains
Almost everyone has twisted their ankle at some in their life; in fact, it is one of the most common reasons for people to visit an emergency department. Technically an ankle sprain has occurred when an ankle twists, causing damage to one of it’s supporting ligaments. The ligaments can be overstretched, partially torn or completely ruptured, depending on the force of the injury. The ligament that is most often involved is the ATFL, or the anterior-talofibular ligament, located on the outside of the ankle. While there are many ligaments surrounding and supporting the ankle, this ligament is the most vulnerable as it stops the ankle from rolling inwards, which is the way that most ankles are injured. Athletes who jump while moving in different directions, such as basketball players, are the most prone to this injury as they often land on their foot when it is not completely flat, twisting it and injuring the ligaments.
What are the signs and symptoms?
Most people won’t have any problem diagnosing that they have a sprained ankle. The symptoms are pain, swelling and tenderness over the area of damage, usually the outside of the ankle. Depending on the severity of the injury, there many be bruising, reduced range of movement, instability and pain with weight bearing. In more severe injuries there may even be a loss of function, where you are unable to walk on the ankle and numbness and/or a feeling of coldness in the foot. Physiotherapy Treatment for Ankle Sprains Twisted ankles can also cause a fracture of the ankle, not just ligament damage and many times a bad sprain and a fracture cannot be told apart without proper medical assessment and an X-ray. Your physiotherapist is able to identify if your sprain is severe enough to need further investigation to rule out a fracture. They will also classify the severity of the sprain, providing you with a clear course of treatment. There are many factors that can lead someone to be more prone to fractures, including general hyper flexibility, unsupportive footwear and anatomical structure, however by far the most common reason for an ankle sprain is the existence of a previous sprain without complete rehabilitation. This is because following an ankle sprain, many people are left with weakness, instability or stiffness, reduced balance and proprioception – which is a sense of where your body is positioned. These things can mean that the next time your ankle is in a vulnerable position you don’t have the strength, awareness of position, balance or structural control to ensure it is in the correct position before putting all your weight through it, causing another injury. As well as helping you reduce and recover from the pain and swelling of the injury in the early days. Your physiotherapist is trained to identify which issues are likely to affect you in the future and assist you with a personalized rehabilitation program to ensure your ankle is as strong and stable as possible to prevent future injuries. Ankle Exercises on the Bosu Ball Here are some of our favourite ankle exercises to do on a bosu ball. All you’re going to need for this exercise is a bosu ball. Preferably practice this exercise without shoes that way it challenges your muscles a bit more. Place 1 leg on the bosu ball and try to balance that for as long as you can. Once this gets a little bit easy for you, you can start to make it a bit more challenging by moving the opposite leg in different directions, sideways or even across. Overtime you will find that your ankle muscles get a bit stronger.
What is it patellofemoral pain syndrome (PFPS)?
Our knees are complex joints, designed to provide stability from side to side and smooth movement forwards and back as you walk, kick and run. The patella, or kneecap, is a small bone embedded in the tendon of the quadriceps muscle that protects the knee and also provides extra leverage to the quadriceps, amplifying their strength. The patella moves up and down in a groove at the front of the knee as the knee bends and straightens. Usually this movement is smooth, with little friction, however, occasionally the soft tissue between the kneecap and the knee can become irritated, causing pain in a typical pattern. This condition is often referred to as ‘runner’s knee’, PFJ Syndrome or patellofemoral pain syndrome (PFPS).it. What causes patellofemoral pain? The patella usually sits in a balanced position in the shallow groove at the front of the knee and moves easily without friction. The patella is attached to the quadriceps muscle at the top and connected to the lower leg via the patella tendon at the bottom. When the quadriceps contracts, this pulls on the patella and acts to straighten the knee. There's a number of factors which play an important role on how the patella, quadriceps tendon and surrounding soft tissue is loaded. Commonly we see people with deconditioned gluteal muscles or overpronating feet who end up suffering from patellar pain. But it's important to understand that on their own these aren't necessarily harmful characteristics. What normally ends up triggering pain is the load that we are putting our knees through and whether they can withstand those loads. Often this all starts with training load errors or badly planned training regimes.
What are the symptoms?
This condition is characterized by pain felt around the patella with activities that require repetitive bending of the knee. The pain may be on the inner side, outer side or underneath the patella. There may be a sensation of, clicking or grinding and some people report that their knee suddenly gives way. The pain is commonly felt when running, going up and down stairs or when doing squats and is relieved with rest. The pain may start as a small niggle and gradually become worse over time. How can physiotherapy help with Patellofemoral pain? The first step in effective treatment is to exclude any other conditions and have a physiotherapist confirm the diagnosis. Your physiotherapist is able to determine which factors are contributing to this condition, which could include poor posture, a lack of arch support in your feet or poor running technique. Once these factors have been identified, you will be provided with a specific treatment program to best approach your condition. PFP syndrome is usually an overloading injury so it responds well to load management strategies like relative rest and progressive reloading. Biomechanical analysis and correction of any muscular weakness may also be important. Having the correct shoes and orthotics can also make a huge difference. There are some short-term treatments, such as patella taping and manual therapy which may help alleviate symptoms quickly and keep you active while you address the other factors contributing to your pain.
Many people know the value that physiotherapy brings to their life and some have even been visiting their physiotherapist since childhood. However, for those who have never been to see a physiotherapist before, there can be a question mark over exactly what it is that physiotherapists do. In fact, this is one of the most common questions physiotherapists are asked.
The answer is tricky, because physiotherapists do so much. Primarily, we might be described as pain management experts, as we work to reduce the pain of our patients, from those who have suffered a new injury, to those who have had pain for several years. We first identify the cause of the pain and then provide manual therapy techniques, education and management strategies to help our patient understand, manage and reduce their pain. While pain is usually the first thing that brings patients to see a physiotherapist, this pain has often caused patients to give up activities that they love and can even be getting in the way of everyday tasks. Many of us reduce our activity levels to reduce pain without even realizing it. Physiotherapists are able to identify which areas you are struggling in and why this is occurring. By identifying the cause of your symptoms, we can help to get you back to full function. Physiotherapists are able to do this for everyone including elite athletes and those dealing with serious disabilities. In fact, physiotherapists have a role to play at practically every stage of life. We can assess infants to monitor their motor skills development and as they grow we help them deal with the pains and vulnerabilities of a growing body. Among other things, we can help improve the function of athletes, assist in preventing injuries, help those with pelvic floor dysfunction and work to prevent falls in the elderly. Not just manual therapy Physiotherapists offer a range of treatments, from targeted stretches, manual therapies, dry needling, exercises and massage. Physiotherapists are also committed educators and take our role as such seriously. A huge part of recovering from pain and injury comes from understanding what is happening and how to best manage these issues. Rather than create a dependency on their therapist, we aim to empower our patients to improve their health independently as much as possible. Physiotherapists aim, to improve your quality of life and remove any barriers to full participation, whether these barriers are due to pain, weakness or stiffness.
Here are some quick tips on how to fast track your progress onto your first pull up or chin up.
- Starting on a step or just jumping to the top of the pull up, holding the position and slowly lowering down, as slow and controlled as you can all the way to the bottom. - Progress from taking 5 seconds going down, to taking 10 seconds, twice the amount of time, and more time and tension to strengthen all the muscles. - Try to hold yourself at the very top. So, from the start try to pull yourself back up, even if you can’t just really try to pull yourself back up as you are slowly lowering down. These are our top tips for progressing onto your first pull up or chin up. |
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
April 2024
Categories |
|
|
|


 RSS Feed
RSS Feed